March 5, 2024
How Does Our Community Paramedicine Program Work?
Even before a patient is discharged from the hospital, the community paramedicine program kicks into gear.
Case manager Amy Rodriguez meets with patients before they leave the hospital to set a follow-up visit with the community paramedicine program team and assess what patients may need during the recovery process.
“We work with patients ahead of time to plan a home visit,” said Rodriguez. “We let our patients know that the community paramedicine program can help set them up with home health, hospice, social workers, and really anything they need.”
After an initial assessment, the community paramedicine program’s team of advanced practice providers, nurses, paramedics, EMTs, physicians, and a case manager and social worker work with patients to ensure they have the resources they need to recover successfully at home and avoid being readmitted to the hospital. This can include assistance with attending follow-up visits, medication management, or a home visit for patients who may be unable to travel to the clinic.

Katie Pemberton, FNP-C, RN-BC
Nurse Practitioner
“We never want a patient to suffer a setback in their recovery because they can’t make it to the clinic. Caring for patients in their home means that we know they are getting the care they need, and it gives our care teams an opportunity to assess additional needs as well.”
“We never want a patient to suffer a setback in their recovery because they can’t make it to the clinic. Caring for patients in their home means that we know they are getting the care they need, and it gives our care teams an opportunity to assess additional needs as well.”

Katie Pemberton, FNP-C, RN-BC
Nurse Practitioner
From food insecurity to a lack of electricity or air conditioning, the community paramedicine team also can connect patients with services addressing a wide range of needs that could negatively impact care and outcomes.
“We know that patients heal and recover better at home,” said Kristin De Los Santos, BSN, RN, Deaf Smith County Hospital District Medicare wellness center director. “Being able to care for someone in their home helps patients open up more and better communicate their needs, and it allows us to better assess how we can best serve our community.”
The program was awarded the Texas Hospital Association’s highest quality recognition in February 2024 with the Bill Aston Award for Quality. Learn more here.

More about HRMC
Hospital Investments Yield Strong Patient Satisfaction Scores
Data reveals high marks from patients treated at Hereford Regional
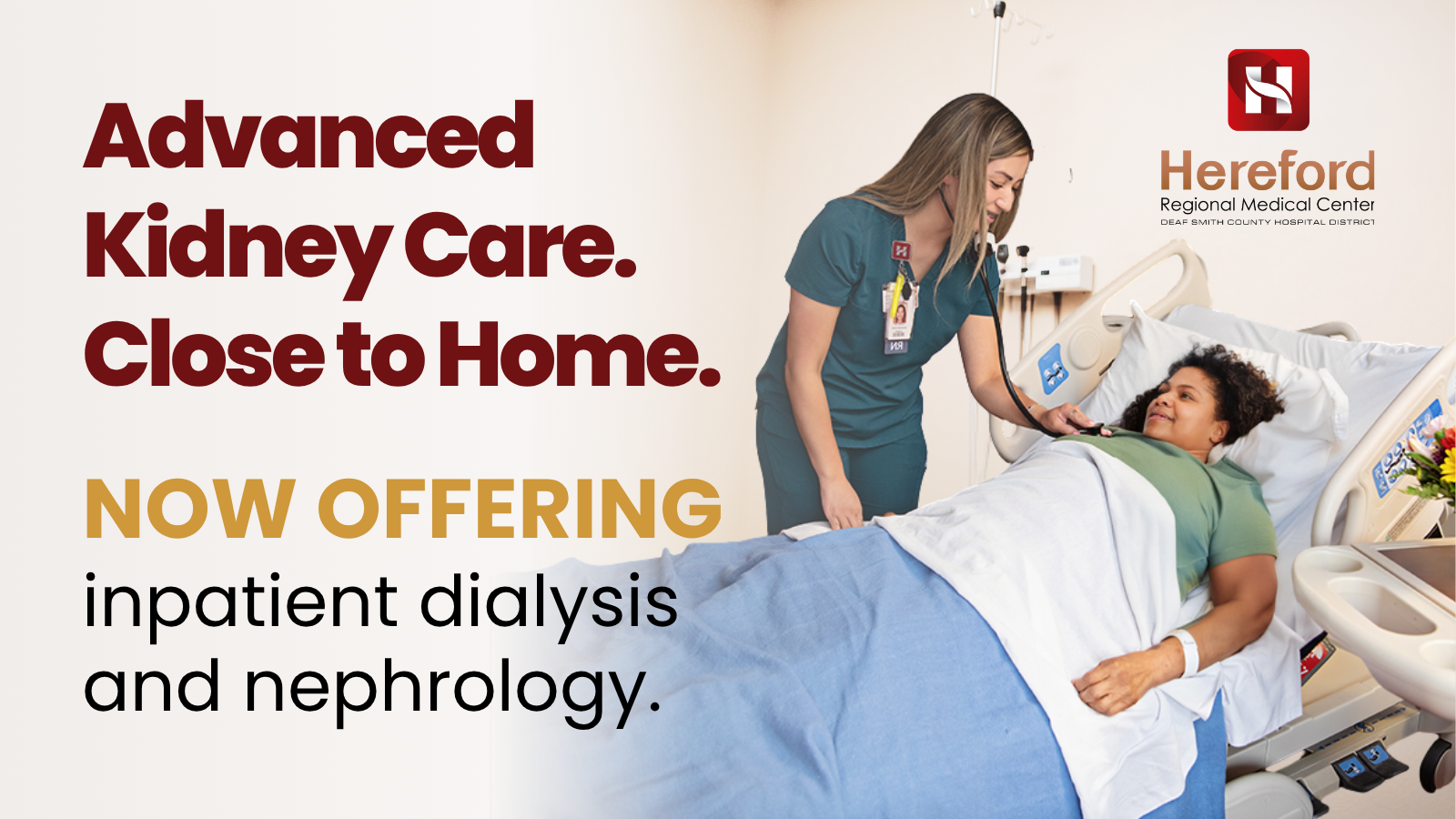
Bringing Kidney Care Closer to Home: How Telemedicine is Changing the Future of Dialysis at HRMC
For many patients living with kidney disease, getting the care
Inpatient Dialysis and Nephrology Services Now Available at Hereford Regional Medical Center
Hereford Regional Medical Center is expanding its specialty services, making