January 22, 2024
Emergency Medical Services’ View of Community Paramedicine
Terry Hazlett is an EMS veteran. Having worked as a paramedic for 40 years, including the past four years as director of EMS for Deaf Smith County Hospital District, there’s not much she hasn’t seen in the course of her career in emergency services.
But, with the launch of DSCHD’s award-winning community paramedicine program in 2022, Terry found herself with a brand-new vision for what is possible for EMS.
The community paramedicine program “has taken my job to a higher level,” she describes. “When I run on a 9-1-1 call now, I don’t look at it as a 9-1-1- call. I look at it as, what can I do beyond offering medical treatment right now? I look at the home, and I start to identify things that we can fix or potentially have the opportunity to fix. And if the patients are not necessarily admitted to our facility, I still follow up and say, how can we help you?”
EMTs and paramedics have a reputation as “adrenaline junkies.” They thrive in environments where most people would be overwhelmed by the chaos and crisis. They are first responders. First on the scene after an accident, crash, or emergency.

Terry Hazlett | DSCHD EMS Director

Brady Moberly | DSCHD EMT
Brady Moberly, one of DSCHD’s emergency medical technicians who is studying to be a paramedic, started assisting Terry when she did home visits as part of the community paramedicine program. When he first started with the program, he admitted he was a bit hesitant because the home visits weren’t like the usual EMT/EMS services. “It’s way different from lights and sirens, 9-1-1, go hurry, there’s a wreck or something,” said Brady.
But, like Terry, Brady quickly saw that even though the setting and services may be different, the role of the EMT in the community paramedicine program is essential. “You use your skills and your knowledge and everything to make a really big difference for the various patients. You’re there to help and encourage them to allow you in and open up to you a little bit, especially in the comfort zone of their home.”
And the impact is significant. “One of the biggest things we’ve seen is keeping people out of the hospital instead of being brought back within a short period of time and having to be readmitted,” said Brady.
DSCHD’s community paramedicine program serves as a model for reducing preventable hospital readmissions by integrating case management, social work, emergency medical services, wellness, and clinic providers into a holistic model of post-discharge care. Working together, the community paramedicine team ensures that every patient discharged gets a home visit, has transportation to clinic visits, receives needed medications, and gets connected with any other needed community or social services, such as Meals on Wheels. In one year, the hospital’s readmission rate fell from a high of 35 percent to 5 percent and improved to a rate of .003 percent between March and September of 2023.

Hereford EMS team

Hereford Regional Medical Center emergency vehicle

Community paramedicine team conducting a home visit
More about HRMC
Flu Cases Are Rising. There’s Still Time to Get Vaccinated.
Flu activity is increasing across the country, and Texas is
Hospital Investments Yield Strong Patient Satisfaction Scores
Data reveals high marks from patients treated at Hereford Regional
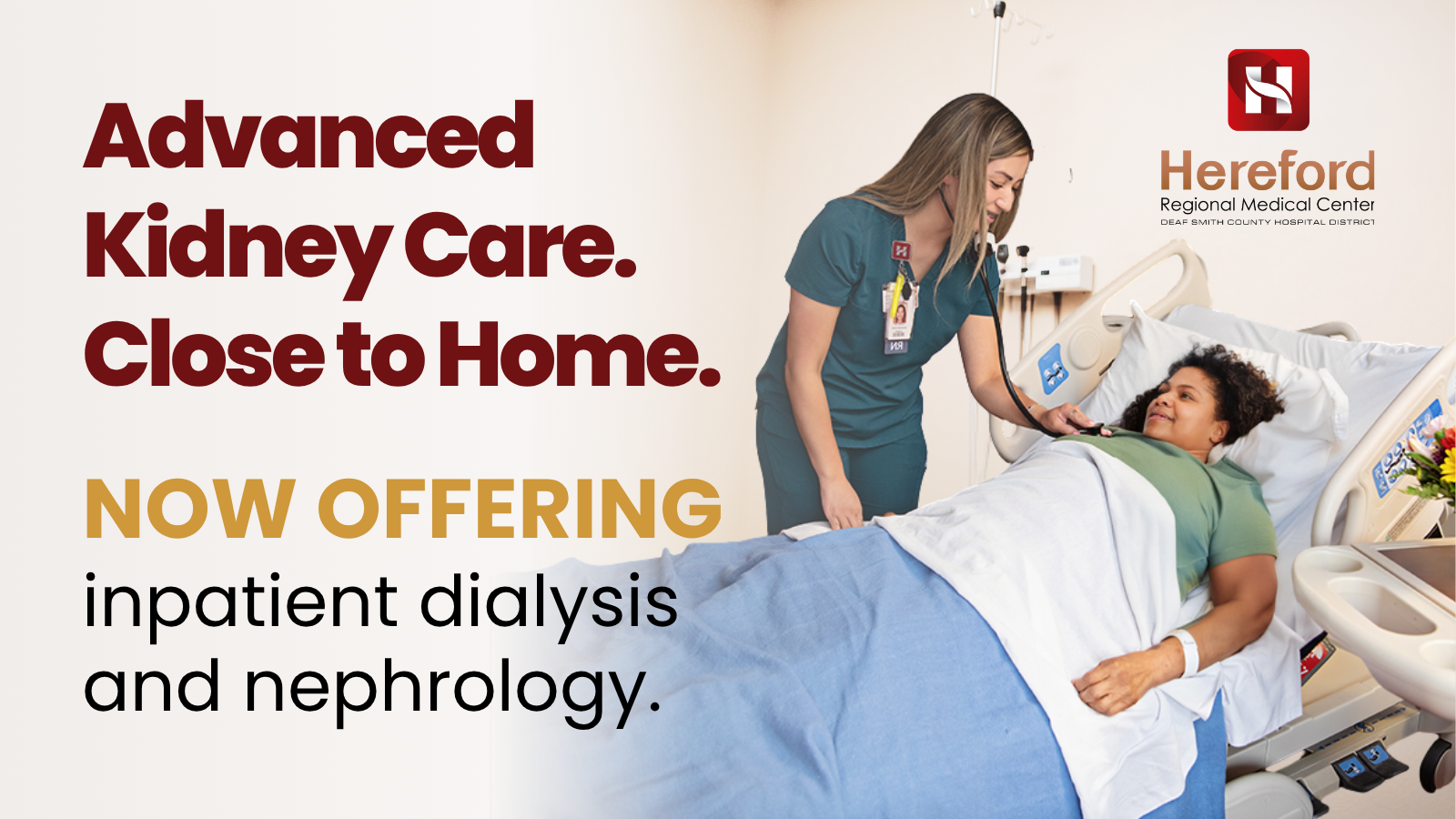
Bringing Kidney Care Closer to Home: How Telemedicine is Changing the Future of Dialysis at HRMC
For many patients living with kidney disease, getting the care